Spreading HIV, the virus that causes AIDS, is against the law in 37 states – with penalties ranging up to life in prison
Despite the fact that HIV is now a treatable medical condition, the majority of U.S. states still have laws on the books that criminalize exposing other people to HIV. Whether or not the virus is transmitted does not matter. Neither does a person’s intention to cause harm. A person simply must be aware of being HIV-positive to be found guilty.
These laws are enforced mainly on marginalized people living in poverty who cannot afford lawyers. The penalties – felony convictions and being placed on sex offender registries – are severe and life altering.
It is difficult to know exactly how many people are affected by HIV criminal laws, since a central database of such arrests does not exist. The HIV Justice Network has collected a partial list of 2,923 HIV criminal cases since 2008 based on media reports.
I am a professor of social work who studies the impact of HIV criminal laws from the perspective of people who have been arrested. My research shows such statutes are outdated, harm people living with HIV and exacerbate the spread of the virus by driving people into hiding and away from treatment services.
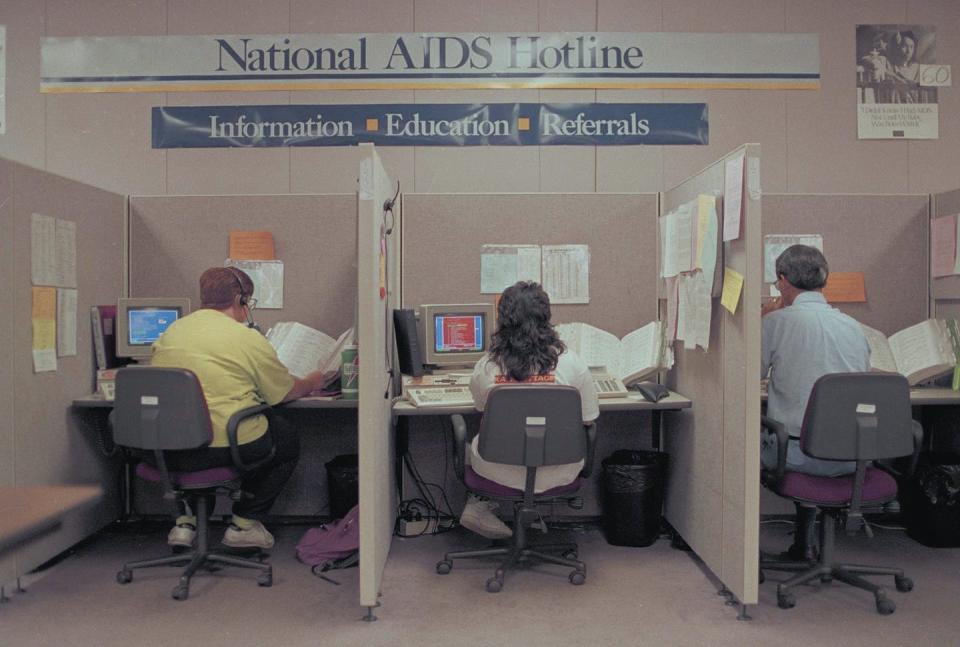
The early years of AIDS
In 1981, the U.S. Centers for Disease Control and Prevention reported the first cases of what later would be called acquired immune deficiency syndrome, or AIDS. By 1982, researchers had strong evidence the disease could be transmitted through blood and sexual activity. At the time, the death rate for AIDS patients was estimated to be 65%.
In 1983, scientists discovered the retrovirus that causes AIDS and named it the human immunodeficiency virus, or HIV. Initially, HIV infection was reported mainly in gay men, but as time went on, it was diagnosed in other populations, including women and children.
In 1994, AIDS was the leading cause of death for all Americans ages 25 to 44. Medical treatment for the disease was in its infancy. Both factors fueled the public’s fear of being exposed to AIDS. A diagnosis seemed like a death sentence.
Criminal laws
The 1988, Ronald Reagan’s Presidential Commission on the HIV Epidemic recommended that states establish criminal penalties as a way of deterring people with HIV from engaging in behavior likely to transmit the virus. The 1990 Ryan White CARE Act, which provided major funding for HIV services, required states to certify they had adequate laws in place to prosecute individuals who knowingly exposed another person to HIV.
In 1990, 14 states had HIV criminal laws. By 2005, 23 states had them – even though the reauthorization of the Ryan White CARE Act in 2000 removed the criminalization requirement. Today, these laws are on the books in 37 states.
Unintended consequences
From the outset, experts across many disciplines voiced concern about the effectiveness of using punitive criminal laws as a way of deterring the spread of HIV.
Indeed, HIV criminal laws have backfired from a public health perspective. A 2017 study found people living in states with HIV criminal laws are less likely to get tested and know their HIV status than those in states without HIV laws. Stigma and fear of prosecution discourage people from seeking information or help.
This lack of knowledge is significant because pharmaceutical treatments, beginning in 1996 with highly active antiretroviral therapy, or HAART, have steadily transformed HIV into a chronic manageable condition.
Medical experts have recommended that HIV criminal laws be revised. However, most state legislatures have not done so.
These laws are regularly enforced – most often on members of stigmatized groups, including those who are homeless or suffering from an addiction or mental illness. Research has also documented that HIV criminal laws are disproportionately applied to people of color. In fact, the majority of people arrested for an HIV crime are members of multiple minority communities.
Being arrested for an HIV-related crime is often devastating for individuals – beginning with the permanent exposure of personal health information to the public. For indigent defendants, felony charges pursued by a county’s district attorney will result in the appointment of a public defender, who will most likely counsel a guilty plea – regardless of whether the individuals believe they are guilty or even understand the consequences of such a plea.
Sentences for violating HIV exposure statutes are comparable to sentences for vehicular homicide and can be as severe as life in prison. A 2017 analysis of 393 convictions in Arkansas, Florida, Louisiana, Michigan, Missouri and Tennessee found the average sentence for an HIV-related crime was 92 months – or nearly eight years in prison.
Incarceration can result in permanent restrictions on employment, housing, education and voting.
Additionally, six states currently place people convicted of an HIV-related crime on the sex offender registry, which results in lifetime sex offender status – a relentless and unending punishment.
Treatment lowers risk
The HIV epidemic in the U.S. has changed tremendously in the past 40 years.
HIV exposure laws have not kept up with the changes in HIV science and treatment. People with knowledge of their HIV status can receive treatment that makes them unable to transmit the virus. Proven prevention methods such as HIV testing, treatment and preexposure prophylaxis, or PrEP, are tools that remove the justification for HIV criminal laws.
Scientists can identify solutions to public health challenges, but it takes action by politicians to turn solutions into policy. HIV criminal laws are largely ignored because the people they directly affect are not connected to political power.
Bipartisan support is needed to replace existing laws with proven public health interventions.
[Get the best of The Conversation, every weekend. Sign up for our weekly newsletter.]
This article is republished from The Conversation, a nonprofit news site dedicated to sharing ideas from academic experts. It was written by: Robin Lennon-Dearing, University of Memphis.
Read more:
Robin Lennon-Dearing has recieved funding from the University of Memphis Foundation and currently receives funding from the National Institutes of Health under Grant 2P30AI042853-21. She is a member and consultant for the Tennessee HIV Modernization Coalition.