Teens with severe obesity are turning to surgery and new weight loss drugs
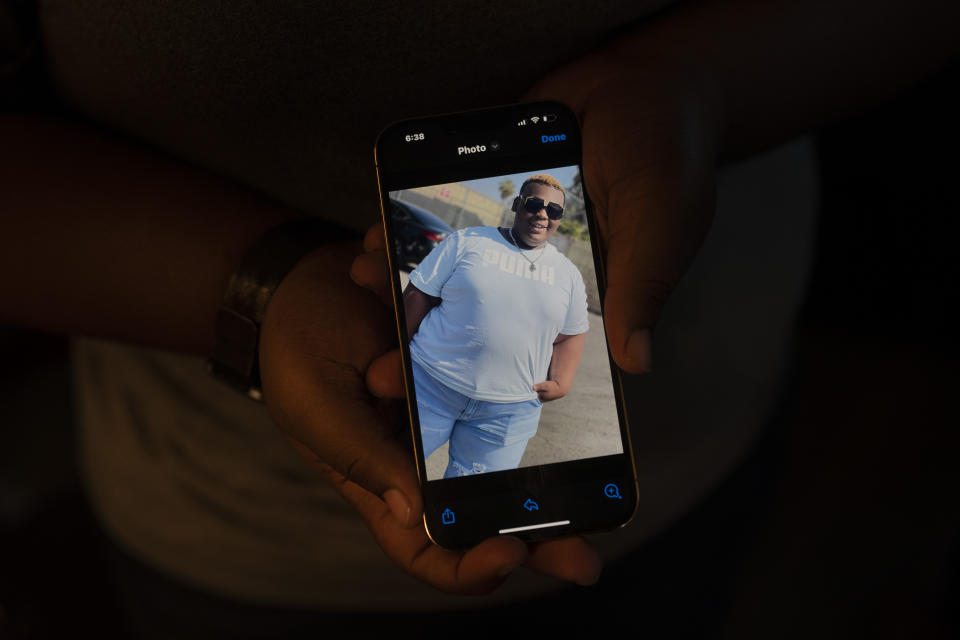
John Simon III was a hungry baby, a “chunky” toddler and a chubby little boy, his mother said. But by age 14, his weight had soared to 430 pounds and was a life-threatening medical condition.
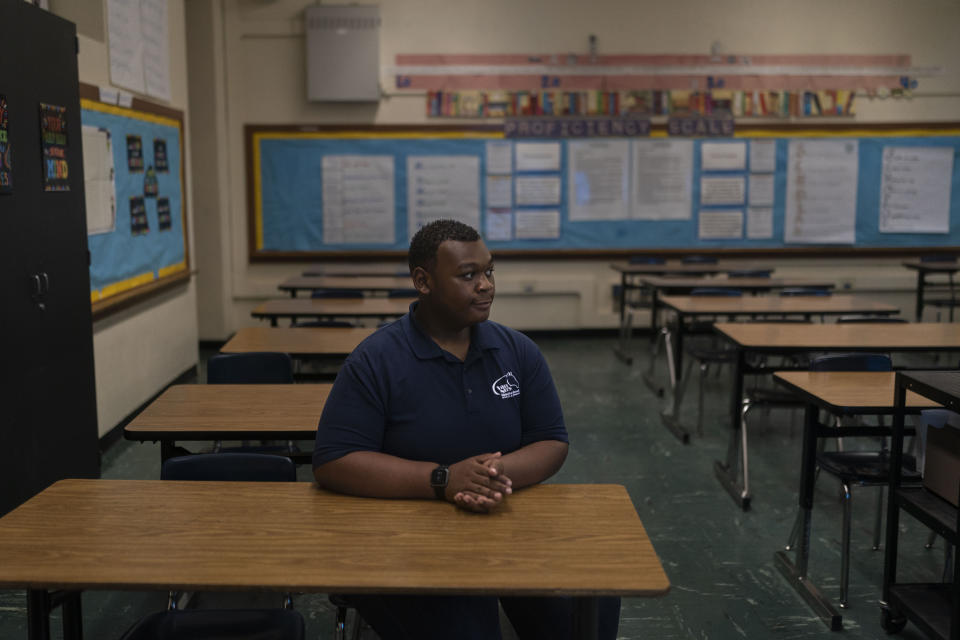
Nine months after weight-loss surgery that removed a portion of his stomach, John has lost about 150 pounds, boosting his health — and his hopes for the future.
“It was like a whole new start,” said John, who will start high school in California this fall.
In Minnesota, Edward Kent was diagnosed with fatty liver disease. The 6-foot, 300-pound high school sophomore started using the obesity drug Wegovy in January — just a month after federal regulators approved it for children 12 and older — and has lost 40 pounds.
“It’s a huge deal and it will affect him for the rest of his life,” said his mother, Dr. Barbara Van Eeckhout, an obstetrician-gynecologist. “This is about his health.”
John and Edward are among a small but growing group of young teens turning to treatments like body-altering surgery and new drugs that rewire metabolism to lose large amounts of weight. Critics urge caution at intervening so early, but the kids and their parents say the aggressive — and often costly — measures are necessary options after years of ineffective diet and exercise programs.
“John has tried with all of his might,” said his mother, Karen Tillman, 46, an accountant. “It’s not because he couldn’t try. It was getting harder and harder.”
Eighty percent of adolescents with excess weight carry it into adulthood, with potentially dire consequences for their health and longevity. Obesity was first classified as a complex, chronic disease a decade ago by the American Medical Association, but meaningful treatments have lagged far behind, said Aaron Kelly, co-director of the Center for Pediatric Obesity Medicine at the University of Minnesota.
“It's a biologically driven disease. It's not a behavioral disease,” Kelly said. “We need to get on it early. Don't wait until later in life because it's too late.”
In January, the American Academy of Pediatrics issued guidelines that call for considering obesity drugs for kids as young as 12 and surgery for those as young as 13. The recommendations were immediately controversial.
Mental Health America, an advocacy group, called them "dangerous” and “disheartening,” saying they would increase eating disorders and perpetuate harmful stigma regarding weight. Some on social media accused doctors and parents of taking the easy way out, blaming things like junk food or video games — or accusing parents of “child abuse.”
Dr. David Ludwig, an endocrinologist and researcher at Boston Children’s Hospital, warned that the “justified excitement” over new weight-loss medications shouldn’t eclipse non-drug options.
“Especially for children, diet and exercise must remain at the forefront of obesity prevention and treatment,” he wrote in JAMA.
But medical experts who treat kids with severe obesity say research is clear: Diet and exercise alone aren't enough. More than 240 diseases are associated with excess weight — including liver problems, diabetes and inflammation — and the signs show up early, said Dr. Janey Pratt, a Stanford University surgeon who performed surgery on John Simon.
“It’s already affecting major organs by the time they get to me,” Pratt said. “You’re dealing with a train that’s headed over a cliff.”
Starting in elementary school, John struggled with joint pain, shortness of breath and sleep apnea so severe that, at age 12, he needed coffee to stay awake. He developed anxiety triggered by daily bullying at school and was hospitalized as a sixth grader for two months with post-traumatic stress disorder.
“They call me names, hit me, push me, all of the above,” John said. “It was a lot of hardship I had to go through.”
He tried diets and exercise, losing up to 40 pounds. But intense food cravings meant the weight always came back — plus more. By the time John met Dr. Callum Rowe, a pediatrics resident in a public health clinic at Children’s Hospital, Los Angeles, John had a body mass index of 75. It was way off of the charts that measure body-mass index, or BMI, which is regarded as a flawed tool but widely used by doctors to screen for obesity.
John, who has a shy smile and a soft voice, asked for help. He said he wanted to go on a “journey to wellness,” Rowe recalled.
“I found that very profound for a 13-year-old. He’s an old soul to have that level of insight about what can I do to change my situation?” said Rowe, who referred John to the Stanford Medicine Children’s Health weight-loss program.
It meant traveling to Palo Alto, 350 miles north, but Karen Tillman said she was ready to do anything.
“His weight was just going up by the minute,” she said.
Sign-ups for the Stanford surgery program have doubled since the release of the AAP guidelines, Pratt said. It's is among the busiest sites in the U.S., performing more than 50 of the 2,000 pediatric weight-loss surgeries logged each year.
John was fortunate; fewer than 1% of children who qualify for metabolic surgery go through with the procedure. Doctors can be reluctant to refer, and families either don't know it's an option or it costs too much, experts said. Fees run upwards of $20,000 and can be as much as $100,000.
John’s surgery was covered by Medi-Cal, California’s Medicaid program, which paid for 47 operations for kids ages 11 to 17 last year, according to state health records. Across the U.S., Medicaid coverage of weight-loss surgery for kids varies significantly by state.
On average, children who receive weight-loss surgery lose about a quarter to a third of their body weight, studies show. But about 25% of kids regain the pounds and need further treatment, Pratt said.
With Wegovy, adolescents lost about 16% of their body mass over nearly 16 months in a clinical trial. Those who take obesity drugs — requests for which have soared at Stanford and nationwide — regain weight once they stop, research shows. Some taking the drugs see potentially serious side effects like gallstones and inflammation of the pancreas.
Edward Kent has responded well to the obesity medication, which has turned off his ravenous appetite “like a light switch,” his mother said. At a recent exam, Edward’s liver function had returned to normal.
John Simon has lost about 35% of his body weight in less than a year. His liver function and insulin resistance have both improved, Pratt said. His arthritis is receding. He’s sleeping better and moving more easily.
John's struggle still extends past conquering cravings and improving his health. Attacks by bullies got so bad at his middle school, teachers were assigned to walk with him between classes.
“He's going to come out with some type of hurt," said John's pastor, Charles Griffin III of DaySpring Christian Church. "The prayer is that when he does come out of this, he will be stronger.”
John graduated this month from his middle school, where officials wouldn’t comment on steps they took to address the bullying. He'll go to a charter high school next year that will be smaller and, his mother hopes, more compassionate.
John, now 15, is focused on the future. He has learned to cook healthy meals, like a recent dinner of sauteed shrimp and chard. He works out at a local gym, puts 18,000 steps on his pedometer every day and hopes to study hard to land his dream job as an automotive engineer.
“I just want to live a happy, healthy life,” he said. “Without the pain. And just without the weight.”
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.