What Is POTS? Explaining the Syndrome Affecting Christina Applegate’s Daughter Sadie
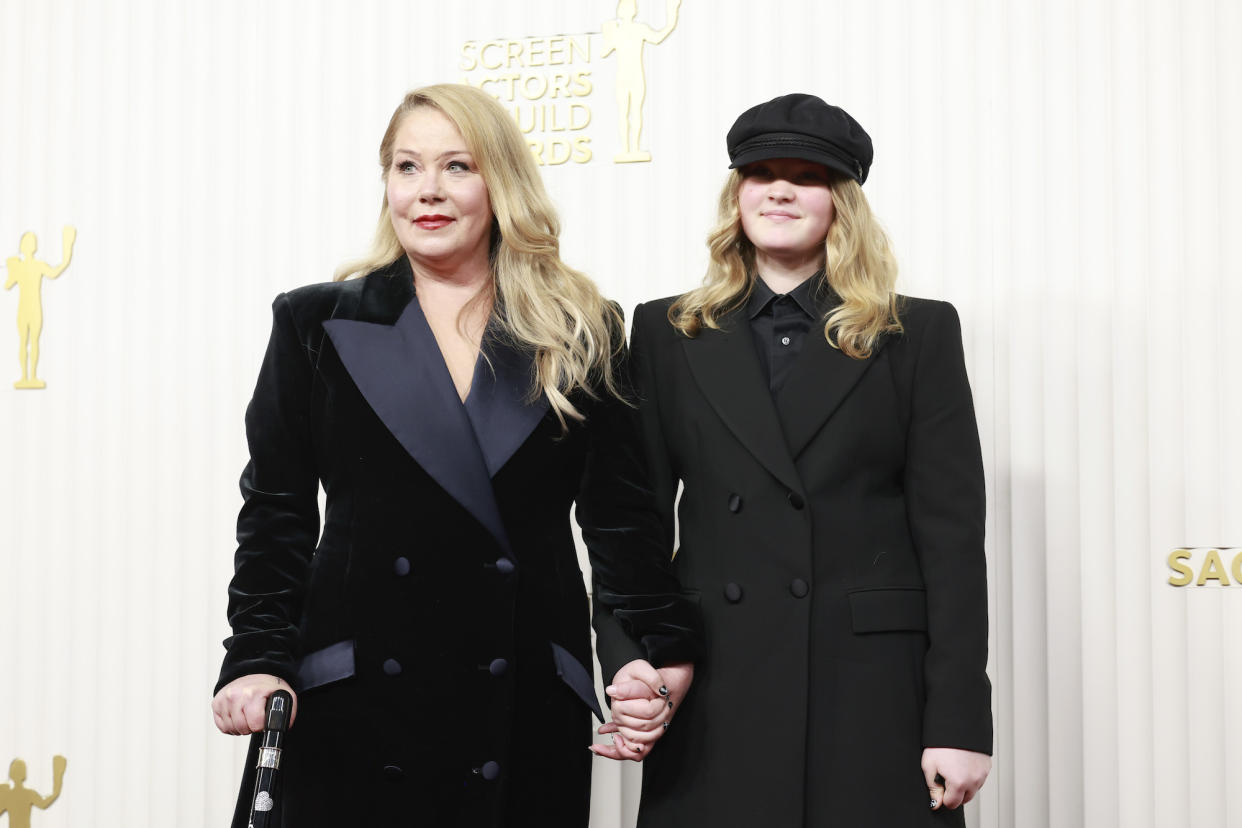
Christina Applegate’s daughter, Sadie, made headlines when she revealed her POTS diagnosis.
“I have something called POTS,” Sadie said on a June 2024 episode of her mom’s “MeSsy” podcast, referring to postural orthostatic tachycardia syndrome. “I have no clue what it actually is but it’s something to do with the autonomic nervous system and it affects my heart. When I stand up, I get really, really dizzy and my legs get really weak and I feel like I’m going to pass out.”
The Dead to Me star — who shares Sadie with her husband, Martyn LeNoble — expressed her sadness for her daughter amid her health battle.
“I hate it for you my darling. I really hate it for you,” she said. “I’m sad. But I love you and I know you’re going to be OK. And I’m here for you and I believe you. And thank you for bringing this to light and awareness.”
According to Dr. Ernst von Schwarz, POTS is not a rare condition. The doctor exclusively told Us Weekly while discussing his book, The Secrets of Immortality, that the disorder affects one in 3 million Americans, particularly young women.
“85% are young women of child beyond age,” the board certified cardiologist said. “Those patients have a reactive hypertension, meaning the blood pressure drops upon changing position, like from getting up from a chair or from the bed, blood pressure drops, the heart rate shoots up, it becomes tachycardic and that then creates lack of oxygen in the brain.”
As a result, von Schwarz explained that “people feel dizzy, lighthead” and might “pass out.”
Scroll down to learn more about the condition:

What Are Symptoms of POTS?
While POTS is not life-threatening, it can be “very annoying” to those who suffer from the condition, he said.
“Those people can have those dizziness episodes 20, 30, 50 times a day,” von Schwarz said. “So it's most likely an autoimmune condition and neurogenic dysfunction, meaning the nerves don't do what they're supposed to do by constricting the blood vessels.”
In addition to dizziness, look out for lightheadedness and palpitations, von Schwarz said. “They feel the heart is racing out of nowhere, and that's a scary feeling,” he said, adding that some people think they’re having a heart attack. “It's really something uncomfortable.”
In some cases, people will pass out or have “extreme vertigo or dizziness” which may limit their daily work or social activities.
Celebrity Health Scares Through the Years
What Are Treatment Options for POTS?
It’s difficult to treat POTS because “everybody reacts different,” von Schwarz said. “The main issue is that there is an intravascular hypervolemia, meaning there's not enough fluid in the body. The vascular system lacks fluid,” von Schwarz explained.
He noted that hydration is critical, but in some instances, it’s not enough to solely drink water. (BTW: water should include electrolytes.)
“But I have several patients in my practice who require on a weekly basis, two, three times intravenous infusions for several hours because they just can't keep up with drinking enough, keep the intravascular volume status high enough,” he said.
Aside from water, von Schwarz encourages patients not to get up too quickly. “If you jump up, the blood vessels dilate, the blood sucks into the lower extremities, there's not enough blood going into the brain,” he continued. “Get up slowly, move your legs, move your feet, use what we call the muscle pumps first before you jump up.”
There are also other options, including medication, von Schwarz added.
Can Patients Grow Out of POTS?
Yes and no, according to von Schwarz. “There were two studies published over the last three to five years, which showed that actually most POTS patients suffer from it for a long, prolonged period of time, meaning several years,” he explained.
However, when a patient becomes older, von Schwarz noted that blood vessels do not dilate as much so the symptoms can “go away.” He added, “So with advanced ages, we don't see the symptoms.”
Are There Any Tricks to Help With POTS Symptoms?
Exercise can help train the blood vessel reactivity, as well as exposing the patient to different temperatures, he said.
“If you take a shower, for example, just don't take a hot shower. Take a shower, hot, cold, hot cold, but always end with cold,” von Schwarz said. “If you end with hot, you might get out of the shower and pass out. So you end with cold because the cold water on the body, it's a constriction of the blood vessels, the blood pressure goes up.”
Does POTS Present Itself With Other Illnesses?
Since POTS is an autoimmune disease, it is “more frequently” seen in people with Lupus or connective tissue diseases, von Schwarz said. “It doesn't mean that every POTS patient will have another autoimmune disease, but there's an increased frequency and we always have to look out for those,” he added.
How Can Caregivers Help Someone With POTS?
He noted that it’s important to take someone’s symptoms “serious enough.” He added, “We have to treat it. So we have to, of course, respect the patient and the symptoms and also provide appropriate help and support.”
Is POTS Hereditary?
He noted that POTS is not hereditary in a “Mendelian way,” but there is an “increased frequency” among generations who have hypotension, or low blood pressure. (Von Schwarz was referring to the inheritance patterns of genes, a phrase named after Gregor Mendel.)
“The good thing is if you have low blood pressure, you might have those symptoms, but you live long,” von Schwarz said. “Whereas if you have high blood pressure, people with high blood, they feel great and very energetic, but they die in their forties or fifties because of the consequences of high blood pressure.”
When Should Someone See a Doctor If They’re Having Symptoms?
Von Schwarz encouraged someone with symptoms to go to their primary care physician who can check the basics. If nothing arises from the initial visit, he recommended seeing a cardiologist.
“It does require sophisticated diagnostic tool basically to make the diagnosis,” von Schwarz said. “And oftentimes it requires that other causes for similar symptoms are ruled out appropriately.”
With reporting by Christina Garibaldi
