Endometriosis Treatment Options
Illustration by Mira Norian for Verywell Health
Medically reviewed by Sanaz Ghazal, MD
There is currently no cure for endometriosis, a disease in which tissue similar to the lining of the uterus grows outside the uterus, causing pain, infertility, and other symptoms.
Endometriosis treatments may include a combination of:
Self-care
Medication
Surgery
Pelvic physical therapy
Treatments for co-occurring conditions
In this article, learn more about treatments for endometriosis.
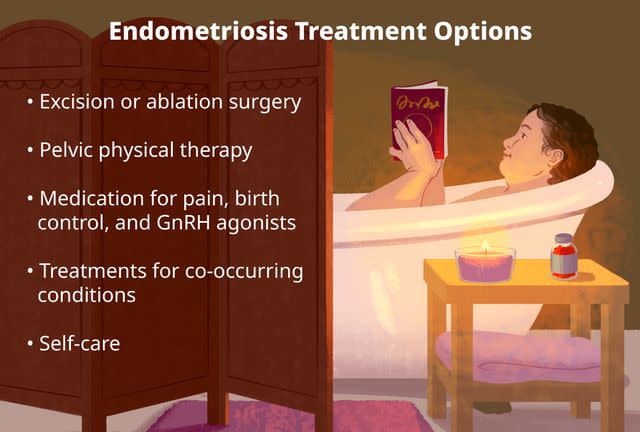
Illustration by Mira Norian for Verywell Health
What Is the Goal of Endometriosis Treatment?
In most cases, the goal of endometriosis treatment is to manage the symptoms associated with the disease and to prevent it from progressing. There are several different approaches to treating endometriosis.
Endometriosis can be associated with pelvic pain, pain with intercourse or bowel movements, and abnormal bleeding. Sometimes the symptoms can be severe and significantly diminish a person's quality of life. There is no cure for endometriosis, but there are ways to manage the symptoms.
For people with endometriosis-related infertility, one goal of treatment may be improving your chances of getting pregnant.
Endometriosis can also cause adhesions (scar tissue) that pull internal organs out of alignment. Another goal of endometriosis surgery is to fix and restore the natural anatomy, which may help both symptoms and fertility.
Factors That Determine Endometriosis Treatment
Not everyone will have the same endometriosis treatment plan. Various factors such as your symptom profile, fertility, health insurance, personal preferences, and more may affect your treatment plan.
In many cases, endometriosis treatment starts with medical management. In more severe cases or when medications are ineffective, excision surgery is another possible option. Surgery for endometriosis is more invasive, costly, and associated with more risks, but it can be very effective in reducing symptoms of endometriosis. Because endometriosis surgery can be complicated, you may want to seek out a doctor that specializes in endometriosis surgery.
It's important to receive full informed consent from your healthcare provider when determining your endometriosis treatment. Discuss all possible side effects or complications from surgery and medications.
Endometriosis Treatment vs. Diagnosis
A definitive endometriosis diagnosis can only come with surgery. Surgeons can resect (cut out) and analyze it through a pathologist to confirm the diagnosis. Removing the tissue implants can both diagnose and offer therapeutic benefits.
Endometriosis Treatment Options
Even though there is no cure for endometriosis, there are several strategies to try to manage the symptoms. These include medical management to help slow down the spread of the disease or decrease symptoms, as well as surgical management to remove endometriotic tissue, resect adhesions or scar tissue, and restore anatomy.
Excision Surgery
If you have severe pelvic pain, gastrointestinal symptoms, infertility, or endometriosis symptoms that are not responding to medical treatment, you may need to consider surgery to excise the endometriosis, remove scar tissue, and restore your internal anatomy.
However, there are few specialists that perform this advanced surgery and some of these specialists are out-of-network with health insurance, which can make access to care more challenging. Oftentimes, these specialists operate with other surgical specialists, such as colorectal surgeons, to perform more complicated surgical cases.
Ablation Surgery
In this more common method of endometriosis surgery, the surface of the lesions is burned rather than removed.
Ablation may involve higher risks of thermal damage to surrounding tissues, higher risk of post-surgery adhesions and pain, and a more significant inflammatory response than excision. A systematic review found ablation was not as effective as excision regarding improvement in pain symptoms one year after surgery.
Pain Medications
If you are hesitant to undergo surgery or have financial barriers to accessing surgical treatment, a healthcare provider may prescribe pain-relieving medications to help you manage your symptoms.
Birth Control
Because endometriosis spread and growth are dependent on hormones, hormonal therapies such as oral contraceptive pills and the progesterone intrauterine device (IUD) can help reduce the symptoms and limit the spread of the disease.
Gonadotropin-Releasing Hormone (GnRH) Agonists
A healthcare provider may recommend the use of gonadotropin-releasing hormone (GnRH) agonists like Lupron Depot (leuprolide acetate for depot suspension), which reduce the hormones by initiating temporary menopause. This can help to reduce symptoms of endometriosis. However, this treatment can have side effects and risks and should be used for a limited duration.
Courses of this treatment are generally limited to between six months and one year due to the risks associated with long-term use including osteoporosis, diabetes, and other metabolic abnormalities.
Pelvic Physical Therapy
This form of physical therapy, which focuses on supporting and retraining the pelvic floor, may be prescribed before endometriosis surgery or during the post-surgery recovery period. Pelvic floor physical therapy can help relieve pain and retrain pelvic muscles, but it does not make endometriosis lesions go away or resolve.
Will You Need Multiple Endometriosis Surgeries?
People who undergo endometriosis surgery may possibly need more than one surgery to address their symptoms. In some cases, endometriosis disease spreads or worsens over time and in other cases when the endometriosis disease remained after incomplete removal or treatment by one surgery. If your disease is more advanced, and you're concerned about needing surgery, see a healthcare provider who specializes in endometriosis.
Treatment for Secondary Endometriosis Conditions
Various health conditions may occur alongside endometriosis or cause similar symptoms. Treatments for endometriosis will not necessarily help these conditions, and your symptoms may continue. Similar conditions and their treatments include:
Adenomyosis: This is often called a "sister condition" to endometriosis, in which the endometrium (the inner layer of the uterus) grows into the uterus muscle wall and causes painful and heavy periods. The definitive cure for adenomyosis is hysterectomy (surgical removal of the uterus). Medications to manage symptoms may be prescribed for those who hope to become pregnant or opt not to have a hysterectomy.
Interstitial cystitis: Also called painful bladder syndrome, this condition may be treated with medications that alleviate pain, reduce urinary frequency, or relax the bladder. Lifestyle changes such as diet adjustments to avoid bladder irritants may also be recommended.
Uterine fibroids: These benign uterus tumors may cause pelvic pain and other symptoms similar to endometriosis. Treatment may include surgery to remove the fibroid, a hysterectomy, medications to manage symptoms, and lifestyle changes.
Does Endometriosis Go Away After a Hysterectomy?
It is an unfortunate myth that a hysterectomy is a treatment for endometriosis. Hysterectomy is a surgery that removes the uterus, and by definition, endometriosis is a disease that exists outside the uterus. Research has also shown that removing the uterus doesn't necessarily lead to better outcomes when compared to excision surgery that spares the uterus.
How Do You Treat Endometriosis at Home?
Many people with endometriosis learn ways to help manage symptoms at home. Some at-home treatments for endometriosis symptoms include:
Applying hot water bottles or electric heat packs
Applying cold packs
Wearing loose clothing without a waistband
Drinking tea (peppermint, spearmint, chamomile, turmeric, or green tea)
Gentle pelvic stretches
Over-the-counter pain medication
Applying topical pain relief or lotions
Massage
Acupuncture
Traditional Chinese medicine
Eating a low-fat, minimally inflammatory diet
Complications of Untreated Endometriosis
Endometriosis can cause debilitating pelvic pain and other symptoms that impact a person's well-being, mental health, and quality of life. Symptoms also affect your financial wellness. Multiple studies have evaluated the economic impact of endometriosis. They show that endometriosis can lead to high healthcare expenses and a lower earned income due to loss of productivity from pelvic pain.
As endometriosis progresses, it can also lead to infertility by creating inflammation and scarring and blocking the fallopian tubes. Endometriosis has also affected fertilization rates and implantation rates as well. It's important to speak with a fertility doctor if you have endometriosis and are trying to get pregnant.
Chronic pelvic pain from endometriosis can also cause long-term issues with the pelvic floor, impacting sex, bowel movements, urination, and more. These muscular imbalances may remain even after surgical lesion removal, though pelvic floor physical therapy can help.
Successful Endometriosis Treatment With a Specialist
If you require endometriosis surgery, working with a surgeon who specializes in endometriosis is important.
Look for an endometriosis excision specialist who is skilled in:
The excision technique
Recognizing all possible colors and appearances of endometriosis
Evaluating the entire pelvic and extra-pelvic area (the rectovaginal space, appendix, bladder, liver, diaphragm, kidneys, intestines, and more)
Summary
Endometriosis treatment includes medical strategies and surgical approaches. Hormonal therapy, pain medications, lifestyle changes, and pelvic physical therapy are often frontline interventions. If your endometriosis symptoms are severe or not responding to minimally invasive strategies, you may consider surgery. If you are, it's important to find a healthcare provider who specializes in endometriosis.
